President Trump’s proposed cuts to the National Institutes of Health (NIH) budget have sparked widespread concern among scientists, healthcare professionals, and policymakers across the nation. As the primary federal agency responsible for medical research funding, the NIH plays a crucial role in advancing treatments and innovations that impact millions of Americans. This article examines the far-reaching trickle-down effects of these significant budget reductions, exploring how they threaten to disrupt ongoing research projects, impede scientific progress, and ultimately affect public health outcomes nationwide.
Impact of NIH Budget Cuts on Medical Research and Public Health Initiatives
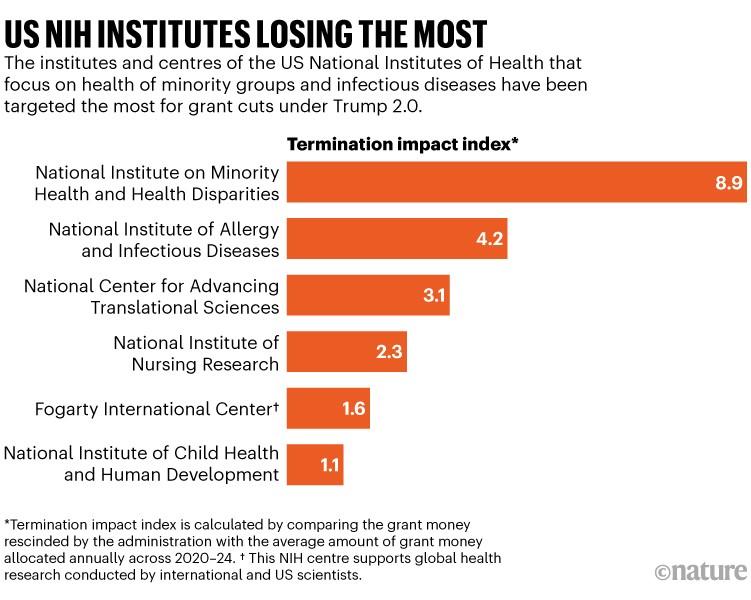
President Trump’s significant reductions in the NIH budget have rattled the very foundation of medical research across the country. Laboratories nationwide have reported slashed funding, forcing many pioneering studies-particularly those in rare diseases and emerging infections-into indefinite delays or cancellations. The immediate fallout extends beyond scientific setbacks; it threatens the pipeline of new treatments and vaccines that rely heavily on NIH grants for initial breakthroughs.
Public health programs, historically sustained by NIH-supported initiatives, are also absorbing the shock. Vital community health efforts targeting cancer prevention, mental health awareness, and epidemic preparedness now face disproportionate cuts. This ripple effect in funding scarcity manifests as:
- Reduced clinical trial opportunities for patients, limiting access to innovative therapies.
- Lower capacity for disease surveillance that hampers early outbreak detection.
- Curtailment of training programs that cultivate the next generation of biomedical scientists.
| Impact Area | Pre-Cut Funding | Post-Cut Estimate |
|---|---|---|
| Rare Disease Research | $120M | $85M |
| Infectious Disease Studies | $250M | $180M |
| Community Health Initiatives | $75M | $50M |
Consequences for Innovation and Long-Term Disease Prevention Efforts
The drastic reduction in NIH funding under President Trump’s administration has led to a noticeable slowdown in medical research innovation across the United States. Laboratories that once thrived on federal grants now face shuttered projects and delayed clinical trials, directly impacting the development of novel therapies and cutting-edge medical devices. This funding squeeze has particularly hurt early-career scientists whose groundbreaking ideas often rely on seed money to get off the ground. As a result, many promising initiatives on the brink of breakthroughs are stalled, jeopardizing future health solutions and technological advancements that could save lives.
Long-term initiatives aimed at preventing chronic diseases such as diabetes, Alzheimer’s, and cardiovascular conditions are also at risk. Prevention programs that depend on consistent funding for research, public health campaigns, and community interventions suffer when budget priorities shift. Without sustained investment, progress slows and the health burden continues to grow. Below is a snapshot of how funding reductions ripple through key areas of disease prevention:
| Area Impacted | Effect of NIH Budget Cuts |
|---|---|
| Chronic Disease Research | Delayed studies, fewer breakthroughs |
| Vaccine Development | Slowed innovation, longer approval times |
| Public Health Programs | Reduced outreach and education efforts |
| Early Career Scientists | Increased attrition, lost talent pipeline |
- Innovation pipelines are disrupted, limiting future treatments.
- Preventative care efforts lose momentum as research findings slow.
- Health disparities risk widening due to lack of sustained intervention.
Strategies for Mitigating Funding Shortfalls and Protecting Scientific Progress
In light of the steep NIH budget reductions, scientific institutions are pivoting to innovative funding approaches that prioritize sustainability amidst fiscal uncertainty. Key policies being adopted include diversifying revenue streams through partnerships with private industry, philanthropic organizations, and international collaborators. Emphasizing efficiency, many research centers are also implementing cost-sharing models and consolidating projects to maintain momentum on high-impact studies despite stricter grant availability.
Beyond financial tactics, safeguarding the integrity of ongoing research depends heavily on strategic workforce planning and resource allocation. Institutions are increasingly focusing on:
- Retaining early-career scientists through targeted fellowships and bridging grants.
- Prioritizing research with clear translational potential to attract alternative funding sources.
- Leveraging data-sharing platforms to reduce duplication and foster collaboration across labs.
| Strategy | Key Benefit | Impact on Research |
|---|---|---|
| Private-Public Partnerships | New capital inflows | Accelerated project funding |
| Cost-Sharing Models | Efficiency in spending | Sustained long-term projects |
| In Summary
As the repercussions of President Trump’s significant NIH budget reductions continue to unfold, experts warn that the trickle-down effects may hamper critical scientific research and innovation across the nation. Funding shortfalls threaten not only immediate projects but also the long-term landscape of medical advancements that countless Americans rely on. Stakeholders across the medical and scientific communities remain vigilant, urging policymakers to consider the broader consequences of these cuts on public health and the country’s leadership in biomedical research. |