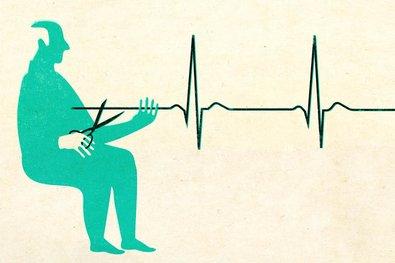
In 2016, Canada made a landmark decision by legalizing medical assistance in dying (MAID), granting terminally ill and suffering citizens the right to end their own lives under strict safeguards. This unprecedented move positioned Canada among a small number of nations embracing assisted dying, sparking intense public debate and ethical reflection. Six years on, The Atlantic examines the profound impact of this legislation-how it has reshaped medical practice, influenced patient autonomy, and challenged societal norms surrounding death and dignity. This article delves into the complex realities that unfolded after Canada gave its citizens the right to die.
Canada’s Journey to Legalizing Medical Assistance in Dying A Closer Look at the Impact on Patients and Healthcare Providers Navigating Ethical Challenges and Policy Recommendations for End-of-Life Care
Since Canada’s landmark decision to legalize Medical Assistance in Dying (MAID) in 2016, the landscape of end-of-life care has undergone profound shifts, impacting both patients and healthcare providers. For many patients facing terminal illnesses or intractable suffering, legal access to MAID has provided a measure of autonomy and relief, allowing them to exert control over their final days. However, the emotional and ethical complexities surrounding the procedure continue to challenge healthcare professionals tasked with balancing compassionate care and moral considerations. Physicians and nurses report navigating a landscape fraught with questions of personal conscience, informed consent, and the evolving definitions of dignity and suffering within clinical practice.
Healthcare institutions across provinces have adapted various policies to support ethical decision-making and safeguard both patients’ rights and providers’ well-being. Key ethical challenges include:
- Ensuring true voluntariness amidst concerns over external pressures or socio-economic factors influencing patient decisions.
- Provider conscientious objection balanced with duties to refer or provide timely access.
- Navigating prognostic uncertainties and eligibility criteria that continue to evolve with legislative amendments.
| Stakeholder | Primary Concern | Policy Recommendation |
|---|---|---|
| Patients | Access equity and informed consent | Improved counseling, standardized information delivery |
| Healthcare Providers | Ethical conflicts, emotional burden | Clear referral pathways, ethics support teams |
| Institutions | Compliance and risk management | Robust oversight, transparent reporting mechanisms |
Insights and Conclusions
As Canada continues to navigate the complex ethical and legal landscape surrounding assisted dying, the experiences since legalization offer critical insights into the evolving relationship between law, medicine, and individual autonomy. While the legislation has provided relief and choice to many facing unbearable suffering, ongoing debates highlight the need for vigilant oversight and continued dialogue. The Canadian case stands as a pivotal example in the global conversation on end-of-life rights, underscoring both the possibilities and challenges inherent in legislating compassion.